Reform Sweden’s healthcare system a comprehensive and equitably funded is frequently cited as a model for universal coverage. The Swedish healthcare system has faced difficulties like rising costs, an aging population, and demands for modernization despite its strengths. This case study looks at recent changes to Sweden’s healthcare system, their motivations, key reform initiatives, and how they changed the healthcare landscape.
An Overview of Sweden’s Healthcare System: Background and Context
The healthcare system in Sweden is primarily financed and managed at the regional level by taxes. It provides free services at the point of use and provides universal coverage to all residents. Primary care, specialist care, and hospital services are the divisions of healthcare services, which are all coordinated to provide comprehensive care.
Problems Solved:
Price Increases: The system’s finances have been strained by rising costs of medical technology and increased demand for healthcare services.
Population Aging: The aging population has increased the demand for elder care and management of chronic diseases.
Inefficiencies: Service delivery inefficiencies and administrative costs are cause for concern.
Equity Problems: There are now disparities in healthcare access and quality between various socioeconomic groups and regions.
Decentralization and regional autonomy are important reform initiatives:
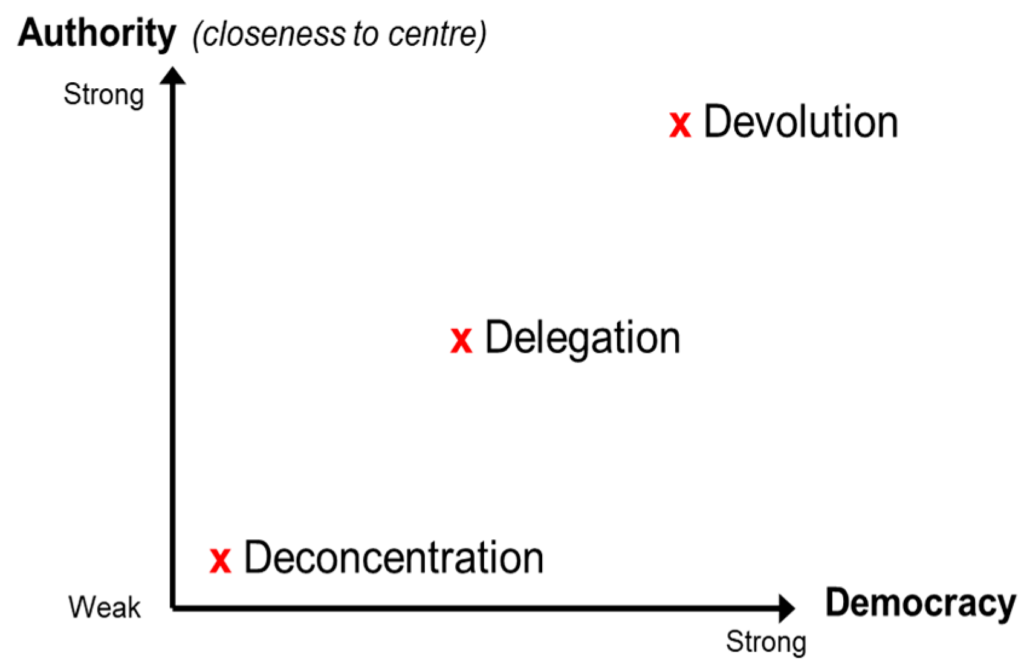
Background: County councils are in charge of providing healthcare in Sweden’s decentralized healthcare system. Regional autonomy has been the focus of recent reforms in order to better meet local needs.
Initiatives: The goal of decentralization efforts is to make regional healthcare management more adaptable. This includes allowing regions to test out new care models and technologies that are tailored to the demographics and requirements of their communities.
Case Study: In order to enhance efficiency and patient outcomes, the Stockholm region has implemented cutting-edge care models like integrated care pathways and digital health services.
E-Health and digitalization:
Background: One of the main goals of reform efforts to modernize healthcare delivery and make it more accessible is to incorporate digital technology.
Initiatives: Telemedicine, patient portals, and electronic health records (EHRs) are examples of digital health solutions that Sweden has invested in. The purpose of these technologies is to facilitate remote consultations, increase patient engagement, and streamline procedures.
Case Study: Patients have access to a digital platform through the “1177 Vrdguiden” service where they can consult with healthcare professionals, book appointments, and get information about healthcare. Access to and efficiency of this system have increased, particularly for non-urgent care.
Preventive and primary care focus:

Background: To lessen the demand for specialist and hospital care, it has been prioritized to strengthen primary care and preventive services.
Initiatives: Through improved coordination and integration with other healthcare services, reforms have aimed to improve primary care services. Preventive health measures are promoted and funding for primary care facilities is being increased as part of the efforts.
Case Study: In order to manage chronic conditions and avoid hospital admissions, the “Close Care” model in Västra Götaland focuses on integrating primary care with community-based services. Patient education and proactive care are emphasized in this model.
Improvements in Quality and Patient-Centered Care:

Background: The agenda for reform centers on ensuring high-quality care and increasing patient satisfaction.
Initiatives: Standards for care, patient feedback mechanisms, and quality measurement systems are some of the reforms. The goal of these measures is to make sure that patient needs are at the center of service delivery and improve the quality of care.
Case Study: In Sweden, the National Board of Health and Welfare has established quality benchmarks and indicators to monitor regional healthcare performance. These indicators assist in promoting accountability and identifying improvement opportunities.
Efficiency and control over costs:
Background: As a response to financial pressures, lowering healthcare costs and increasing efficiency have been major goals.
Initiatives: The implementation of cost-effective technologies, reducing waste, and streamlining administrative procedures are among the efforts. The emphasis has been placed on ensuring that high care standards are maintained while resources are utilized effectively.
Case Study: Patients are able to select their primary care providers from a list of approved options under the “Vrdval” system, which has been implemented in a number of areas. By providing providers with incentives to provide high-quality, cost-effective care, this system aims to increase efficiency while also fostering competition.
Impact of Changes on Accessibility and Convenience:

Accessibility to healthcare services has increased with the introduction of digital health services and improved primary care models. Patients now have easier access to care and better control over chronic conditions.
Increased Productivity:
More streamlined procedures and cost savings have resulted from reforms designed to eliminate inefficiencies. The delivery of services has become more individualized and efficient as a result of healthcare management’s decentralization.
Care Quality:
Improved healthcare outcomes and higher levels of patient satisfaction can be attributed to initiatives that focus on patient-centered care and quality measurement. Better management of chronic diseases has also resulted from the emphasis placed on primary care and prevention.
Problems Remain:
Disparities in access to and quality of healthcare across regions are among the obstacles that remain despite progress. The system is still under financial strain and requires constant modernization.
Future Plans Continuous Innovation:

To meet the needs and challenges of the future, Sweden is likely to keep investing in digital health innovations and investigate novel care models.
Getting Rid of Disparities:
In order to guarantee that everyone in the country has equal access to healthcare, efforts to reduce regional and socioeconomic disparities will be essential.
Cost Control and Sustainability:
The healthcare system’s long-term viability will require constant attention to resource allocation, efficiency, and cost management.
Engagement of Patients:
In order to improve outcomes and increase patient satisfaction, it will be essential to increase patient engagement and participation in healthcare decision-making.
In conclusion,
Sweden’s efforts to reform its healthcare system are a comprehensive strategy for addressing the issues associated with a universal healthcare system. Sweden has made significant progress in enhancing healthcare accessibility, efficiency, and quality through decentralization, digitization, a focus on primary care, and cost-control measures. However, ongoing efforts are required to address remaining obstacles and guarantee the system’s continued effectiveness and viability. The lessons learned by Sweden can be used by other nations that want to modernize and reform their healthcare systems.